The Mini-Heart Revolution
HKU researchers have developed the world’s first human mini-heart, which is radically changing drug discovery and opening up the promise of growing a full-sized, transplantable heart in the laboratory.
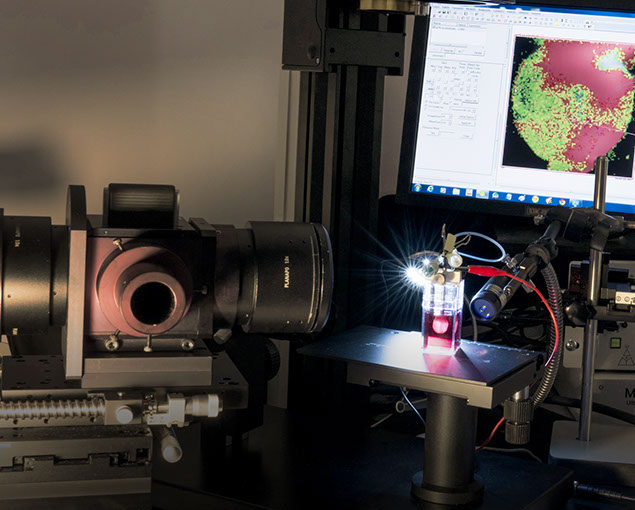
A mini human heart engineered from ventricular heart muscle cells derived from pluripotent stem cells being recorded for electrocardiogram signals or ‘heart rhythms’.

Professor Ronald Li, S Y and H Y Cheng Professor in Stem Cell Biology and Regenerative Medicine, completed his studies in the 1990s with this take-away: “We learned that the heart cannot be regenerated and that when you have a heart attack and the heart cells are gone, they cannot be replaced.”
Today, he is at the forefront of research showing that this seemingly-formidable obstacle can be conquered.
In his native United States, and since 2010 at HKU, Professor Li has been using stem cell technology to regenerate the heart through radical new products, including genetically-engineered heart cells, heart tissues that can act as bandages to repair damage, and a tiny, beating heart that potentially could be developed for human transplantation.
He has overseen the development of these new products with a young, fast-working team at HKU and international collaborators at Johns Hopkins University, Wyss Institute at Harvard, Mount Sinai Hospital and the University of California, Irvine.
In 2010, Professor Li and his team persuaded the Hong Kong Government to adopt ‘Stem Cell’ as one of three health-related topics to be funded under the Theme-based Research Scheme (TRS). The following year they secured TRS funding for their own project and developed the mass production of human heart cells, improving yields from 0.5 per cent to 95 per cent. With sufficient raw materials, they were able to assemble the cells into human heart ‘sheets’ and muscle fibres, and just over a year ago into the 3D mini-heart.

![]() If I take five millilitres of blood from you today, you can come back in three to six months and I will show you a mini-heart pump made from your cells.
If I take five millilitres of blood from you today, you can come back in three to six months and I will show you a mini-heart pump made from your cells. ![]()
Professor Ronald Li
Safer, speedier drug trials
This research is significant not only for heart regeneration, but also, more immediately, for drug research. Many drugs that make it to the clinical trial stage end up being pulled because of cardiotoxicity – whether they are designed for heart conditions or not.
“We think the reason for this is because of the big jump from testing drugs in small animals, like mice and rats, to testing in humans,” he said. “Now, we can use bio-artificial organs instead to screen cardiotoxicity and even discover beneficial effects.”
These discoveries mean that rather than testing one drug at a time in patients, drug companies can test multiple compounds and get much more immediate feedback on the effects.
Pointing to red thimble-sized hearts suspended in jars, Professor Li said: “The mini-heart is our most comprehensive tool. It can measure the pressure-volume relationships, contractility, electrical properties, electrocardiogram (ECG), stress test, pharmacological responses – pretty much everything the cardiologist would measure in the clinic. But it’s not necessarily the best tool for first-level screening because it takes more time. For that we have higher-throughput tools. If you want to look at force, muscle fibres are better. Or if you want to test 50,000 compounds, which we have been asked to do, the miniature ‘hair-like’ heart muscles are more suitable.
“The other thing is that we can test drugs in an ethnic-specific and disease-specific manner which takes into account genetic differences that result in side effects.”

A bio-artifical human cardiac ventricular chamber or mini-heart.
Personalised treatment
Professor Li is also working with international colleagues to create a system of multiple crucial organs that would be a ‘virtual’ human for clinical trials.
Having introduced these revolutionary tools into drug discovery, the next goal is to develop the prototypes into personalised treatment for patients. This is already very close to reality.
“If I take five millilitres of blood from you today, you can come back in three to six months and I will show you a mini-heart pump made from your cells,” he said. “One of our first mini-hearts belongs to an anonymous team member in the laboratory.”
But while the science is progressing rapidly, there are political and other non-scientific obstacles to stem cell-derived products. Some countries, such as Japan, are more forward-looking than others.
“I am often asked when we will be able to generate a whole heart. It’s an academic question we will continue to address, but for patients to benefit, I don’t think we have to wait to fabricate a whole heart. Just a patch can be put on a patient’s heart and if that is sufficient to slow down or stop the disease from progressing, it already does most of the job.”
For the record, three to five years seems a likely horizon for developing a whole heart in the laboratory. In the meantime, Professor Li’s start-up, Novoheart, is working with the drug industry to put the mini-heart and other engineered constructs to use in drug discovery. “Now that we have cells to work with as fundamental building blocks, we can go in and engineer them. It opens up a lot of possibilities,” said Professor Li.
Next

