BRINGING HOPE FOR CONGENITAL DISORDERS
Discovering your baby has an incurable inherited disorder can have a lifelong psychological, social and economic impact on families. But new insights into the molecular genetic bases of two such disorders – Hirschsprung disease and dwarfism – hold promise for developing therapies to lessen the impact. Moreover, the findings may have implications for understanding common disorders that affect millions of people globally.
Back
Hirschsprung disease is a congenital affliction in which babies are born with a bowel that lacks nerve cells to control movement along the gut. The only option for treatment is to surgically remove the affected part of the bowel. But about one-third to one-half of these babies will then suffer lifelong residual problems such as enterocolitis (a potentially life-threatening infection of the bowel), chronic constipation, incontinence and, for a small number, the inability to absorb nutrients.
Professor Paul Tam Kwong-hang, Li Shu-Pui Professor in Surgery and Chair Professor of Paediatric Surgery, is a world-leading expert on the disease and has received multiple honours for his work, most recently becoming the first Asian recipient of the Rehbein Medal from the European Paediatric Surgeons’ Association. He has studied the disease for more than three decades, motivated by the impact of the disease itself as well as by its prevalence in Asian populations, where it affects one in 3,000 births against the global average of one in 5,000 births.
“The problem with Hirschsprung disease and its treatment is that it can affect patients’ future social behaviour, their educational accomplishments and other activities throughout their lives,” he said. “We overlooked these hidden disabilities in the past and the parents were usually just very grateful that we saved the life of their baby. But if you dig deeper, you can see they need more help. Their child’s long-term survival has come at some cost.”
In order to improve that situation, better understanding of the disease is needed so better treatments can be developed. Professor Tam and his colleagues have focussed on genetic studies and stem cell investigations to find answers.
Alzheimer’s link
Over the past decade, they conducted the first whole-genome genetic screening of Hirschsprung disease and identified a single gene that can cause the disease in 10 per cent of cases. They also unravelled some of the genetic complexities involved in the other 90 per cent of cases.
“We have come to realise that it’s not just one gene but a constellation of changes in different genes that can cause this disease, and that the disease will be different in different patients,” said Dr Maria Mercedes Garcia-Barcelo, Associate Professor of Surgery. “This means that a group of genes that lead to the disorder in patient A are going to be different from the group affecting patient B, and they will have different outcomes. Nonetheless, we know there is usually going to be more than one gene involved.”
The team has also showed that mutations can affect the different pathways involved in bowel development. One pathway tells cells to migrate down the spinal cord to the gut, another tells the gut cells to differentiate into neurons, and a third tells these cells to divide and multiply.
Last year, they also identified an additional pathway related to cell survival: even if cells reach their destinations and become neurons, they can still die due to an abnormal build-up of protein that suffocates the cell. The genetic basis of this action was discovered by Dr Clara Tang, Research Assistant Professor in the Department of Surgery, who also found it had wider implications beyond Hirschsprung disease.
“This is a similar, overlapping mechanism to what we see in Alzheimer’s disease. Interestingly, Alzheimer’s patients can also have intestinal problems that cause constipation,” she said.
Stem cell potential
The team’s work has pointed to possible options for treatment, particularly with stem cells. If a patient’s own cells can be re-engineered through induced pluripotent stem cell treatment and placed back in the patient, this conceivably could address the genetic defects. However, further research will be needed first.
The genetic studies of Hirschsprung disease are also uncovering other disease susceptibilities in patients with the disease, which could improve their outcomes from those diseases. For instance, the researchers found that a tiny percentage of Hirschsprung patients carry another genetic defect that makes them more susceptible to thyroid cancer. Already, they have identified an early-stage tumour in a patient who otherwise had no symptoms.
More genetic information will enable more such links to be found and enable researchers to identify targets for treatment. The team already has whole genome sequences of hundreds of Hirschsprung patients, which have been developed through collaborations with overseas scholars and hospitals in Hong Kong, Mainland China and Vietnam, and they are continuing to add to that pool.
“The lessons we learn from this rare disease can apply to the study of other diseases. Studying rare diseases can provide shortcuts for investigating other more common problems. It is a win-win situation,” Professor Tam said.
Integrated Stress Response
Collagen X needs to fold so it can be transported to the matrix outside cartilage cells, where it normally would provide structural support. But sometimes the cells cannot fold properly and instead accumulate inside the cells. This causes a kind of ‘constipation’ that triggers the Integrated Stress Response (ISR), which ultimately ends up affecting the growth plates that control bone formation.
This happens because the ISR causes a potent factor called SOX9, which controls the ways cartilage cells differentiate, to activate in the late stages of the bone development process when it should be shut off. As a result, bones do not form properly.
Understanding the molecular development of MCDS meant that Professor Cheah and her team could start exploring whether the ISR could be inhibited. They treated pregnant mouse models that reproduced the same MCDS abnormality with a readily-available small molecule known to inhibit the ISR, and found it had a therapeutic effect: the dwarfism was prevented by inhibiting the ISR pathway without other side effects.
“To our delight, when the babies were born, their dwarfism was about 95 per cent corrected and their bones were more normal,” she said.
This offers a potential new pathway for future drug development for human patients who would benefit significantly from even some amelioration of dwarfism. A patent has been filed for the treatment, although this will need more refinement and research before it can be applied in humans.
Little people need help
Nonetheless, after eight years of genetic investigations and deep mechanistic studies using mouse models, there may be hope of treating congenital dwarfism associated with the stress response such as that seen in MCDS.
“For people who are dwarfs, being able to grow an extra inch or two will be incredibly important for them. Little people are teased by other children and in MCDS patients, because their bones are not formed properly, they also have pain from abnormal weight-bearing on their joints,” Professor Cheah said.
Moreover, because activation of the ISR is the hallmark of many common diseases, such as osteoarthritis, spinal disc degeneration and fibrosis in other tissues that involve abnormal synthesis of matrix proteins, the impact of these findings extends beyond congenital dwarfism disorders.
“Our work shows why it’s important to do fundamental research and understand the mechanisms of disease because this is how we find potential routes for treatment,” Professor Cheah said. “It’s like fixing a car – if we don’t know how things work, how can we fix them? And if we only did translational research, we could not acquire this basic knowledge and develop our own intellectual property. It can take many years to reach fruition, but basic research has the power to form a good foundation for future translation. The joy of seeing that the MCDS mouse pups were near normal was
beyond description!”
A potential therapy for dwarfism
Our skeletons provide the essential structural framework to support and protect our bodies from the repeated impact of walking, running and bearing weight. But skeletal disorders are the most frequent causes of severe long-term pain and physical disability. Apart from acquired disorders such as osteoporosis, there are more than 400 types of congenital disorders, many of which may result in malformed bones or dwarfism. Current treatment options for dwarfism are extremely limited, but new research at HKU has highlighted a potential new path of therapy for some patients.
Chair Professor of Biochemistry and Jimmy and Emily Tang Professor in Molecular Genetics, Kathryn Cheah, and her team have discovered the mechanism behind a genetic mutation that causes a certain kind of dwarfism, Metaphyseal chondrodysplasia, Schmid type (MCDS), which is characterised by short limbs and bowed legs, leading to a waddling gait and joint pain. Through this understanding, it may be possible in future to develop effective treatments for dwarfism caused by similar mechanisms.
“Underlying all studies trying to develop drugs for diseases is the fact that you need to know the fundamental mechanism – why a genetic alteration results in that phenotype. Although just one gene is altered, it probably has a ripple effect, so that at the end of the day what you see in the patient is the sum total of all the changes that resulted from that first initiating event,” she said.
With MCDS, the body produces an abnormal form of collagen X, which results in the dwarfism. Professor Cheah’s team showed how this happened.
.jpg?crc=388717768)

![]() We overlooked these hidden disabilities in the past and the parents were usually just very grateful that we saved the life of their baby. But if you dig deeper, you can see they need more help. Their child’s long-term survival has come at some cost.
We overlooked these hidden disabilities in the past and the parents were usually just very grateful that we saved the life of their baby. But if you dig deeper, you can see they need more help. Their child’s long-term survival has come at some cost. ![]()
Professor Paul Tam Kwong-hang
![]() Our work shows why it’s important
Our work shows why it’s important
to do fundamental research and understand the mechanisms of disease because
this is how we find potential routes for treatment. ![]()
Professor Kathryn Cheah

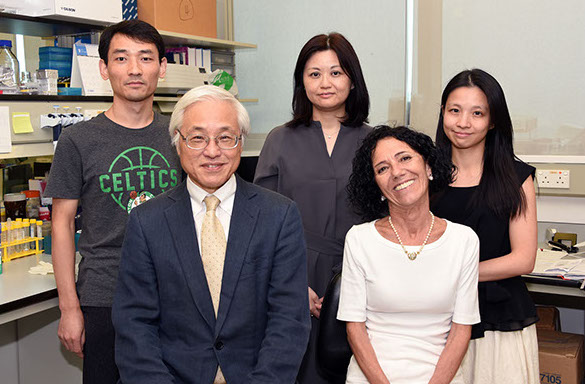
Team members for the research include (back row from left) Dr Li Peng, Dr Elly Ngan, Dr Clara Tang, (front row from left) Professor Paul Tam and Dr Maria Mercedes Garcia-Barcelo.
An HKU-led international team of scientists – (from left) Professor Danny Chan, Dr Maggie Wang, Professor Kathryn Cheah and Dr Tommy Tan – has uncovered why cellular stress can cause dwarfism and provided a therapeutic lead that can be exploited to develop drugs to treat such bone disorders.

Home
May 2019
Volume 20
No. 2
Cover Story
