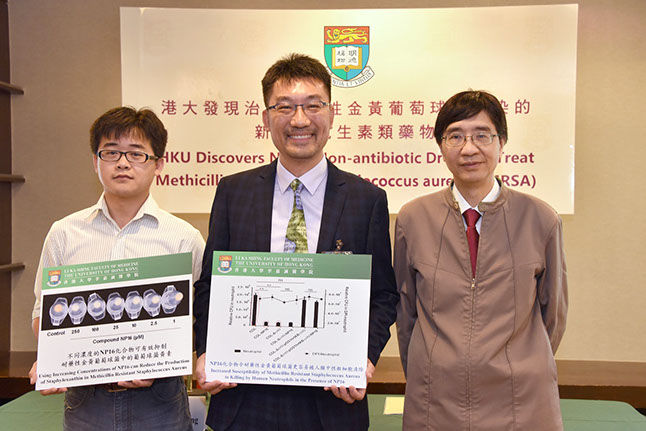
Antibiotic-resistant superbugs kill more than 700,000 people each year and in 2016 the United Nations declared them a threat to global health security. Yet apart from educating doctors not to prescribe antibiotics indiscriminately, and asking patients not to demand them for inappropriate reasons, there have not been effective solutions to the problem. Dr Richard Kao Yi-tsun and his team hope their discovery will be different.
They spent eight years pursuing a line of research that seeks to alter rather than kill off bacteria. Their target was Staphylococcus aureus – a type of bacteria that lives on the skin of 30 per cent of people, becomes harmful when it invades through wounds or other opportunities, and has also evolved the strain methicillin-resistant Staphylococcus aureus (MRSA), a superbug found in most hospitals around the world.
Dr Kao said they were motivated by the simple fact that antibiotics only seem to help resistant forms thrive. “When you use powerful antibiotics, there will always be some that survive because of random mutations in the genome. It might only be one in a billion, but they double in number every 20 minutes so you could very quickly have an antibiotic-resistant population. Basically, antibiotic use may be selecting those bacteria that cannot be killed by that drug,” he said.
Instead, he and his team have deployed a method based on chemical genetics, a relatively new field that uses molecules to change the genomes of organisms.
Their target was the golden pigment of Staphylococcus aureus, which acts as a shield to protect it from attacks by the human immune system, in particular reactive oxygen species (ROS) that are produced by nutrophils and other immune cells. Previous researchers had shown that changing the pigment to white would disarm the shield and make the bacteria vulnerable to ROS.

A lot more competition
Using high throughput screening, they tested 50,000 different compounds and selected several likely candidates for further testing. The best succeeded in turning the golden pigment of Staphylococcus aureus white. “Once the bacteria lose the ability to produce the pigment, they have trouble infecting wounds in humans or animals because the immune cells are able to engulf them. So we’re not changing anything in the body, we are just letting the body do its own work by making the bacteria vulnerable,” he said.
This approach has a major global advantage beyond the health of the host because it could reduce the proliferation of resistant bacteria – a problem that has developed not only from antibiotic prescriptions for health problems but also the widespread use of antibiotics in farming. “Because we are not killing off the bacteria, those that develop antibiotic-resistant become just one in a billion individual bacteria. Otherwise, if you kill off all of their competitors with antibiotics and they become the sole survivors, they will quickly expand into a huge population,” Dr Kao said.
The results were published in the top microbiology journal mBio in September, 2017 and have attracted interest from pharmaceutical companies, who want to explore how to take this laboratory-based discovery to the next stages of testing and turn it into a drug. This will take several years to happen but the first important steps have been taken.
Dr Kao sees their success as an encouraging development for chemical genetics, which he first became interested in nearly two decades ago while doing his post-doc at Harvard. Professor Stuart Schreiber was pioneering the field and one of the people in his laboratory was Professor Dan Yang, who is now Morningside Professor in Chemical Biology and Chair Professor of Chemistry at HKU. She and Dr Kao have become close collaborators in applying chemical genetics to SARS, influenza and bacteria.
“Mainstream research is still trying to find more antibiotics and this is also important. I’m not saying our compound should replace antibiotics, I’m just proposing a new alternative way to let people consider that besides killing bacteria with conventional antibiotics, we can use non-antibiotic compounds to control the disease and not kill the organism. This means less chance of getting resistant bacteria, which is a major advantage. Because we know that when any new antibiotic comes out, very soon afterwards you will have resistant bacteria,” he said.
DISARMING
THE GOLDEN INVADERS
Microbiologist Dr Richard Kao Yi-tsun and his team have developed a novel approach to antibiotic-resistant bacteria that keeps the bugs alive but makes them vulnerable to attack by the human immune system.
Dr Richard Kao Yi-tsun
![]() We can use non-antibiotic compounds to control the disease and not kill the
We can use non-antibiotic compounds to control the disease and not kill the
organism. This means less chance of
getting resistant bacteria, which is a major advantage. Because we know that when
any new antibiotic comes out, very soon afterwards you will have resistant
bacteria. ![]()
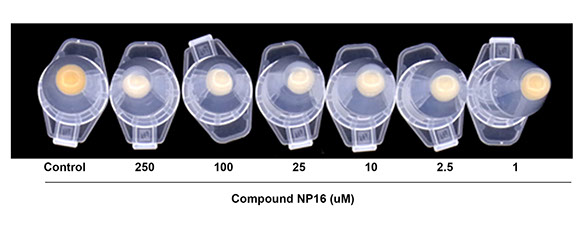
Using increasing concentrations of NP16 can reduce the production of Staphyloxanthin in methicillin-resistant Staphylococcus aureus.
Next
(From left) Dr Gao Peng, Post-doctoral Fellow, Dr Richard Kao Yi-tsun, Associate Professor, and Professor Yuen Kwok-yung, Henry Fok Professor in Infectious Diseases, Chair Professor of Infectious Diseases, Department of Microbiology at the press conference presenting their research findings.